Lumbar Decompression
Posterior Spinal Decompression Surgery for Spinal Stenosis
The following information is intended to give you some general guidelines on what to do after your operation. It is important that you understand what to expect and feel able to take an active role in your treatment. There will be many different health professionals involved in your care during your stay and there will be a clear plan for any after care when you are discharged from hospital. This information will answer some of the questions that you may have, but if there is anything that you or your family are not sure about then please ask Mr Seel or the nurse on the ward.
What is spinal stenosis?
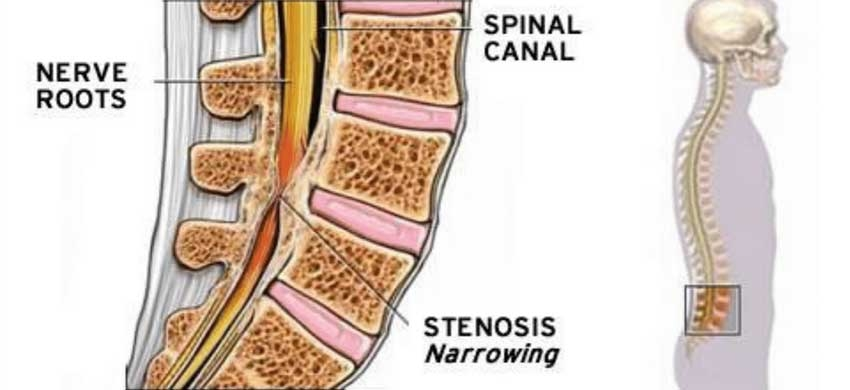
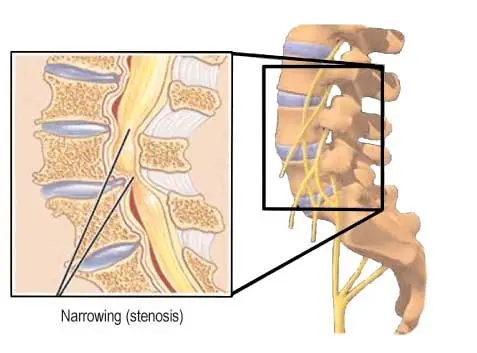
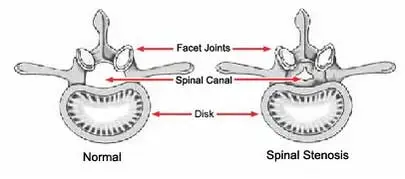
Your spine is made up of many vertebrae with discs between them. The spinal canal is behind this bony column, in which lies your spinal cord and spinal nerves. Holes along the length of the canal allow the nerves to your arms and legs to exit. Stenosis means narrowing of this canal or the exit holes.
What is the treatment?
Spinal decompression surgery is performed under a general anaesthetic (you are asleep) and involves enlarging the space around the nerves so they do not have pressure on them. Surgical treatment is done for those patients with symptoms which prevent them carrying out daily activities. It is mostly done to improve leg pain. The majority of patients who have spinal stenosis have slowly progressive symptoms.
What are the alternatives?
You probably have tried most of the alternatives before considering surgery, they include: gentle exercise and spinal physiotherapy, regular pain relief prescribed by your GP, avoiding heavy and physical activity and a lumbar epidural injection.
Why have I got spinal stenosis?
Posterior spinal decompression surgery is carried out on patients with spinal stenosis. This is a condition where the spinal canal narrows and in turn compresses the spinal cord and/or spinal nerves, which can cause pain, numbness and tingling in the legs. This is commonly due to spinal degeneration that occurs with aging. It can also sometimes be caused by intervertebral disc herniation (“slipped disc”), and rarely by a fracture or a tumour. In the cervical (neck) and lumbar (low back) region it can be a condition people are born with and may vary in severity.
When stenosis occurs in the lower back, it is called lumbar spinal stenosis. It often results from the normal aging process. As people age, the soft tissues and bones in the spine may harden or become overgrown. These degenerative changes may narrow the space around the spinal cord and result in spinal stenosis.
Degenerative changes of the spine are seen in up to 95% of people by the age of 50. Spinal stenosis most often occurs in adults over 60 years old. Pressure on the spinal cord is equally common in men and women, although women are more likely to have symptoms that require treatment.
A small number of people are born with back problems that develop into lumbar spinal stenosis. This is known as congenital spinal stenosis. It occurs most often in men. People usually first notice symptoms between the ages of 30 and 50.
Surgical technique for spinal decompression
A skin incision is made in the midline of the back, dependent on how many levels of your spine are affected. They will remove enough bone and ligament tissue from the back of the spine to free the trapped nerves.
Your surgeon may need to join the bones using a bone graft. Sometimes they made need to use metal screws and rods (a fusion, to stabilise the spine). The operation will last approximately between 1 hour and 2.5 hours but you will be away from the ward longer for longer than this. You will normally stay in hospital between 1 and 3 days following surgery, depending on how quickly you recover.
What are the possible risks or complications of this surgery?
Deep infection – approx. 1 in every 100 cases, you will be given antibiotics into the vein at the time of surgery to minimise this.
Superficial wound infections – 4 in every 100 patients get this and may require a short course of antibiotics.
Bleeding – less than 1 in every 100 patients have a significant bleed, which may require treatment.
Durotomy – the dura is the delicate sac that contains the spinal nerves inside the spinal canal. Occasionally, 1 in 25, this can become snagged or torn inadvertently during the surgery. This can usually be recognised and repaired at the time and would not cause any long term problems, You might have a headache for a couple of days afterwards.
Blood Clots – in the deep veins of the legs or lungs. You will be given surgical stockings and pumps on your legs during surgery to minimise this risk, although we cannot eradicate it.
Sensory change or muscle weakness in legs – is uncommon, approx 1 in 300, when it does occur, it is usually temporary but could be long-standing.
Post-op bladder or bowel dysfunction – The risk of damage to the nerves that supply your bladder and bowel is very rare, < 0.1% (1 in 1000).
Recurrence of Pain – In less than 1 in 100 people the natural process of healing by scar tissue causes pain to return by encasing nerves in too much scar tissue. This is treated by special medications.
Recurrent narrowing – is unlikely, and would take several years to develop.
Repeat surgery – 1 in every 100 patients have further back surgery during the ten years that follow due to continued back degeneration at other levels.
Back pain – Around 1-2 out of every 100 patients develop long term low back pain after spinal decompression, and this can often be treated non-surgically.
For elderly patients some risks are slightly increased. Risk of blood clots, heart attacks, urine/chest infection, and heart failure are all increased with advancing age.
What happens after the operation?
Once you have had your surgery, you will be taken to one of the orthopaedic wards to be looked after for the rest of your stay. You may return from theatre with a ‘drip’ until you are drinking which, if you are able, may be when you come round from the anaesthetic. You may have a PCA (patient controlled analgesia) which provides you with painkillers through a drip tube until you are drinking, and then you will be able to have tablet painkillers. Patients do not tend to have a drain attached (to drain fluid/blood off your wound) but this does occur sometimes. You may have a urinary catheter, which would normally be removed on the first post-operative day.
Immediately after your surgery
If your pain is controlled, you should be able to sit up in bed, and mobilise to the toilet on the evening of the operation, with assistance.
Day following your surgery
With assistance you will be able to mobilise if your surgeon is happy with your progress. A physiotherapist may see you and assist you to move around. Your wound dressing will be changed only as needed and is usually kept covered until the stiches are trimmed at 14 days post-op.
Going home
You will be encouraged to walk and manage stairs as quickly as possible and the ward nurses and physiotherapists will guide you as to how quickly you can go home. This varies between 1 and 3 days after the operation. You will be given a 2 week follow up appointment with Mr Seel for a wound check and to trim your stitches (the rest will be dissolving stitches).
Exercises
You will be given a outpatients physiotherapy appointment between 2-4 weeks after your surgery. Until that point it is important to do your own exercises. Each exercise should be performed ten times, regularly throughout the day. You should start the exercises on the day after your operation and continue them at home.
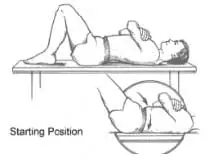
Transversus abdominus

This muscle is a deep support muscle for your spine. Whenever you move it contracts and stabilises the lower spine. Your physio will teach you to locate it. Lying on your back with knees bent and arms by your side. Pull stomach up and in by tightening your pelvic floor muscles/ lower abdominal muscles. Breath normally whilst holding this contraction. Try not to arch your back or push down into the bed. Hold 10 secs, then relax. Repeat 10 times.
Pelvic tilts
Lie on your back with your knees bent up. Gently flatten the small of your back onto the floor and tilt your hips up. Repeat 15 times.
Knee rolls

Lie on your back with your knees bent up. Gently roll the knees from side to side. Don’t push through any pain. Repeat 20 times.
Alternate Leg Hugs

Lying on your back with a cushion under your head. Pull your knee onto your stomach helping with your hands. Push your other leg down towards the floor. Hold approx. 20 secs, then relax. Repeat 5 times on each leg
What will happen after I am discharged?
Pain: Some pain is usual up to the first 2 weeks following surgery. The back pain from surgery will die down to a dull ache after 48 to 72 hours post op. This is usually managed with regular painkillers. Information regarding what to do if you are in undue or extreme pain after surgery can be found here.
Wound care: Your wound dressing will be checked before you leave hospital. You will be given a 2 week follow up appointment with Mr Seel for a wound check and to trim your stitches (the rest will be dissolving stitches). You should keep your wound clean and dry following surgery. Most dressings are shower-proof, but ask your nurse before discharge.
Sitting: You may find that perching on the edge of a bed or perching stool is more comfortable to begin with. You should sit on an upright chair and avoid low chairs or sofas for the first couple of weeks. Try using a lumbar roll or cushion positioned in the small of your back when sitting. Change position regularly, alternating between lying, sitting and walking.
Activity and exercise: Walking is the best activity to do following your surgery. It helps improve your general fitness and leg strength. Gradually build up the amount of walking that you do each day. Try to get into a routine so that you gradually get in the habit of walking a bit further and faster. You may swim as soon as your wound is healed which is normally around 2-3 weeks. Any other sports should be avoided until you can discuss them with Mr Seel in your follow-up appointment.
Heavy lifting and carrying: Should be avoided for the first 4 weeks. Lift weights close to your body, keeping your back as straight as possible and bending your hips and knees to make use of the thigh muscles.
Work: You may return to work as soon as you feel comfortable to do so. If your work involves sitting at a desk you may return to work after about two to three weeks. If you have a heavy job you may need longer to recover (up to 6-8 weeks).
Driving: You will be unable to drive for at least 2 weeks. When considering whether to drive, you have to be able to safely perform an emergency stop, with full pressure on the brake pedal, without significant back/leg pain. Further advice can be sought at your outpatient appointment. Break up long journeys so you can change position and move around. Check with your insurance company as they may wish to know that you have had an operation.
Sex: There is no reason to avoid sexual relations during the recovery period. You might prefer to be the passive partner or try different positions to find the most comfortable for you.
Follow up outpatient appointment: You will be given a 2 week follow up appointment with Mr Seel for a wound check, and a further appointment around 6 weeks after the operation to check your progress. Please discuss any queries you may have when you are at the clinic. Further outpatient appointments are made as necessary. You will also be followed up with a physiotherapy outpatients appointment between 2-3 weeks following surgery.